June 9, 2020
Acoustics + Physical Health
Acoustics - Physical Health Research Brief
Summary
Acoustics can have significant effect on physical health. Quality acoustics can improve health outcomes for hospital staff as well as patients and their families. Poor acoustics, however, can negatively impact sleep and recovery rates, and contribute to long-term health outcomes such as cardiovascular disease and noise-induced hearing loss.
Overview
I. General Physiological Impacts
Much like daylight and other environmental phenomena, acoustics can have significant effect on physical health. Agreeable acoustic conditions with a balance of silence and noise can improve health outcomes for hospital staff as well as patients and their families. Poor acoustics, however, can negatively impact physical health. Infants in the NICU may exhibit decreased oxygen saturation, elevated blood pressure, increased heart and respiration rate, an worsened sleep; high noise exposure may also cause increased awakenings, sleep loss, and sleep fragmentation in adults; constant noise exposure increases rate of patient rehospitalization and medication; noise induced hearing loss and occupational induced hearing loss are increasingly common in industrialized communities. (Basner 2014 1326. 1330)
II. Improved Health Outcomes
The introduction of music into the hospital space can elicit positive emotions and induce an analgesic effect, reducing stress, blood pressure and post-operative trauma when matched with silence, as shown in the figure below (Iyendo 2016). When ambient hospital sounds, such as beeping machines and wailing alarms, are masked and music or television is played quietly, social connection between staff, patients and their families is more commonly reported (ibid). When all facility users feel calm, healthy, and connected they operate as a team, making treatment more holistic.
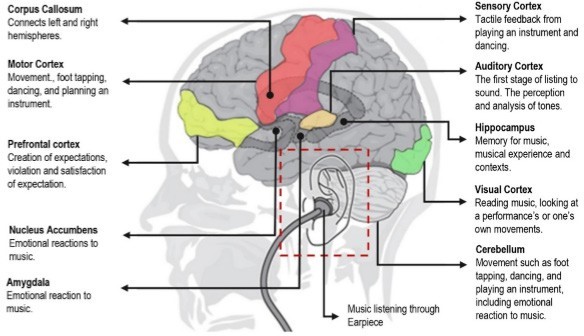
Functional neuroimagining studies on music and emotion suggest that music can modulate activity in brain structures that are known to be crucially involved in emotion (Iyendo 2016).
III. Effects on Sleep
High noise has contributed to increased sleep loss and awakening and sleep fragmentation, with sounds as low as 33bD able to induce physiological reactions during sleep including autonomic, motor, and cortical arousal (eg. tachycardia, body movements, and awakening). Short-term noise induced sleep disturbance include impaired mood, subjectively and objectively increased daytime sleepiness, and impaired cognitive performance. Elderly people, children, shift-workers, and people with a pre-existing (sleep) disorder are thought of as at-risk groups for noise-induced sleep disturbance. Repeated noise-induced arousals interfere with sleep quality through changes in sleep structure, which include delayed sleep onset and early awakenings, reduced deep (slow-wave) and rapid eye movement sleep, and an increase in time spent awake and in superficial sleep stages. This nocturnal noise exposure may be a larger contributor to long-term health outcomes like cardiovascular disease than daytime noise exposure (Basner 2014).
IV. Impacts on At-risk Populations
Neonates, long-term patients, and elderly people are thought to be particularly at-risk to the effects of noise. The sound environment in hospitals, especially in intensive care units, can be characterised by irregularly occurring noises from sources such as medical devices (eg, alarms and beeping), telephones or pagers, conversations, door sounds, and nursing activities. Such noise worsens patient health outcomes through factors such as increased cardiovascular stress, longer healing times, increases in doses of pain-relief drugs, and increased patient readmission rates (Basner 2014).
V. Impacts on At-risk Populations
A study of patients with coronary artery disease found that “there was a significantly higher frequency for the need of extra intravenous beta-blockers in the group during bad acoustics rehospitalization rate at 3 months was significantly higher in the group of bad acoustics, it could not be excluded that this also may have a negative impact on the rehabilitation period,” (Hagerman 2005).
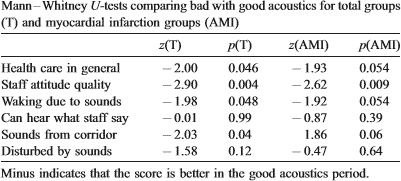
The results of the comparisons between groups of hospital patients in “good” and “bad” acoustics conditions (Hagerman 2005).
VI. Noise-induced Hearing Loss
Global Burden of Disease 2010 estimated that 1.3 billion people are affected by hearing loss and investigators rated hearing loss as the 13th most important contributor (19.9 million years, 2.6% of total number) to the global years lived with disability (YLD) (Basner 2014, 1325).
Although noise-induced hearing loss is well recognised in industrial settings like construction and manufacturing, individuals with other occupations such as musicians, those working in the military, or aeronautics also contribute substantially to the overall burden of noise-induced hearing loss. Noise levels in hospitals are now typically more than LAeq 15–20 dB higher than those recommended by WHO. Hospital noise could therefore be an increasing threat to patient rehabilitation and staff performance (Basner 1326, 1330).
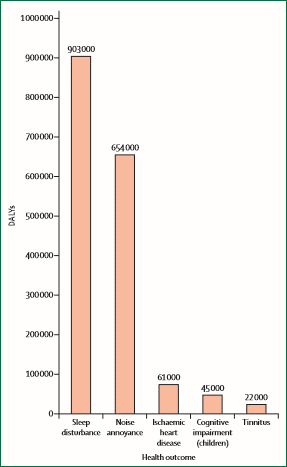
DALYs attributed to environmental noise exposure in Europe. According to World Health Organization, more than 1 million healthy life years (DALYs) are lost annually because of environmental noise exposure in European A-member states alone. Most of these DALYs can be attributed to noise-induced sleep disturbance and annoyance (Basner 2014).
VII. References
Review Articles
- Basner, Mathias, Wolfgang Babisch, Adrian Davis, Mark Brink, Charlotte Clark, Sabine Janssen, and Stephen Stansfeld. “Auditory and non-auditory effects of noise on health.” The Lancet 383, no. 9925 (2014): 1325-1332.
- Hagerman, Inger, Gundars Rasmanis, Vanja Blomkvist, Roger Ulrich, Claire Anne Eriksen, and Töres Theorell. “Influence of intensive coronary care acoustics on the quality of care and physiological state of patients.” International journal of cardiology 98, no. 2 (2005): 267-270.
- Iyendo, Timothy Onosahwo. “Exploring the effect of sound and music on health in hospital settings: A narrative review.” International journal of nursing studies 63 (2016): 82-100.
Primary Research
- Eriksson, Charlotta, Mats E. Nilsson, Saskia M. Willers, Lars Gidhagen, Tom Bellander, and Göran Pershagen. “Traffic noise and cardiovascular health in Sweden: The roadside study.” Noise and Health 14, no. 59 (2012): 140.
- Fuchs, H. V., X. Zha, and H. Drotleff. “Relevance and treatment of the low frequency domain for noise control and acoustic comfort in rooms.” Acta Acustica united with Acustica91, no. 5 (2005): 920-928.
- Fredriksson, Ann-Charlotte, Leif Hellström, and Ulrica Nilsson. “Patients’ perception of music versus ordinary sound in a post-anaesthesia care unit: a randomised crossover trial.” Intensive and Critical Care Nursing 25, no. 4 (2009): 208-213.
- Thorgaard, Bitten, Birgitte Brøndsted Henriksen, Gunhild Pedersbæk, and Inger Thomsen. “Specially selected music in the cardiac laboratory—an important tool for improvement of the wellbeing of patients.” European Journal of Cardiovascular Nursing 3, no. 1 (2004): 21-26.
- Van Kamp, Irene, and Hugh Davies. “Noise and health in vulnerable groups: a review.” Noise and health 15, no. 64 (2013): 153.
Popular Press
- “Noise Exposure is Becoming ‘the new secondhand smoke’”– The Washington Post
- “A Healthy Return: The Business Case for Well-Being in the Workplace”– Metrolpois Magazine
- “A Sound Plan: How to Achieve Optimal Healthcare Acoustics” – Healthcare Design Magazine